Does a Family History of Breast Cancer Mean You Will Get It?
Having a family history increases risk but does not guarantee breast cancer. Most women with affected relatives never develop the disease. Early screening significantly lowers risk through timely detection.
It’s a quiet Sunday morning at your home. You’re sipping tea with your mother.
She mentions her elder sister—your aunt—who passed away from breast cancer ten years ago. “Should you get checked?” she asks softly.
If breast cancer runs in your family, this question is natural. And the answer is not as frightening as it sounds.
Today’s blog talks about the family history of breast cancer, the real risks and what tests to take.
Let’s dive in.
When Does Family History Actually Signal Higher Breast Cancer Risk?
Risk rises if close relatives were diagnosed before age 50, if multiple family members are affected, or if cancer occurred in both breasts. These patterns suggest possible hereditary risk and require medical evaluation.

In families, stories of illness pass quietly between generations. Sometimes, they carry fear; sometimes, they bring strength.
Having a family history of breast cancer does not mean cancer is inevitable. It means your risk is higher—and timing matters.
Medical experts watch for patterns that raise red flags, not coincidences:
- A mother or sister diagnosed before age 50
- Cancer occurring in both breasts
- Multiple close relatives on the same side of the family affected
These signals aren’t meant to scare. They exist to catch risk before it becomes reality.
And here’s what many don’t know: only 5-10% of all breast cancers are truly hereditary. [Source]
The rest happens due to age, lifestyle, and random cell changes.
Is “Family History” the Same as “Hereditary” Breast Cancer?
Family history of breast cancer reflects shared risk patterns, while hereditary breast cancer is caused by inherited genetic mutations that significantly increase lifetime cancer risk.
A family history of breast cancer means cancer has occurred in relatives. Usually due to age, lifestyle, hormonal exposure, or environment.
- Risk is moderately increased.
- Cancer tends to appear later in life
- And, management focuses on earlier or more frequent screening.
Hereditary breast cancer occurs when a pathogenic gene mutation is inherited, impairing DNA repair from birth.
- Risk is high and predictable.
- Cancer often develops at a younger age
- May affect multiple generations and both sexes
- Requires genetic counselling and preventive strategies.
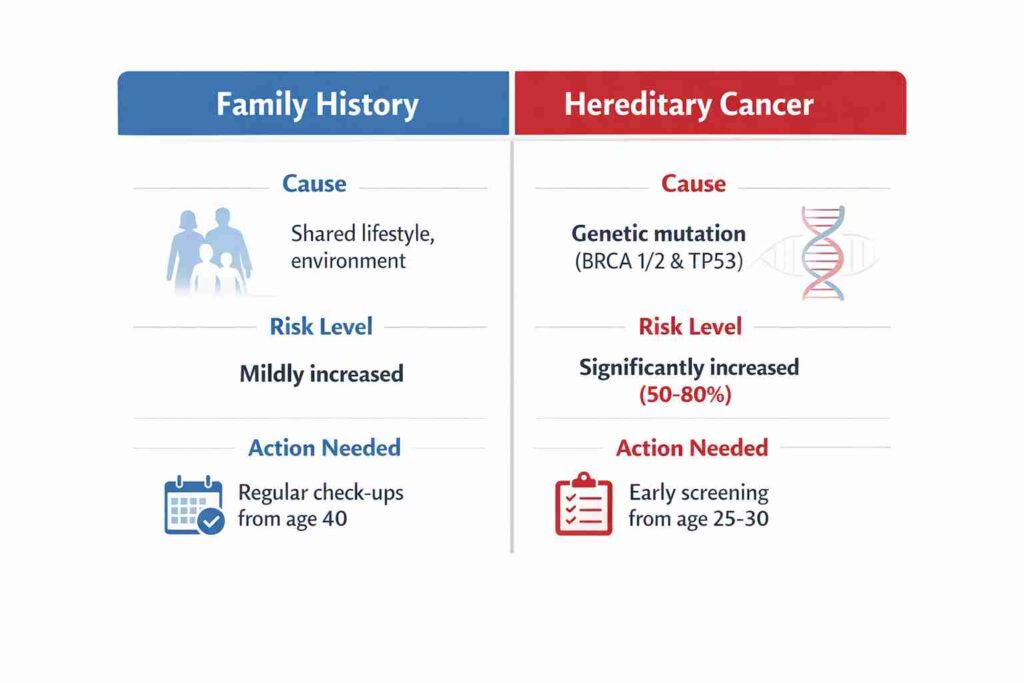
Knowing the difference can replace fear with clarity. That’s where your breast cancer doctor in Kolkata becomes your lifelong guide.
What Are the Real Breast Cancer Risk Factors Beyond Genetics?
Age, hormonal exposure, weight after menopause, alcohol use, and physical inactivity contribute more to breast cancer risk than genetics for most women.
Age and Hormones:
- Risk increases after 40 (Source)
- Early periods (before 12) or late menopause (after 55)
- Never having children or a first child after 30
Lifestyle Factors:
- Being overweight, especially after menopause
- Drinking alcohol regularly
- Smoking and lack of physical activity
Genetic Factors:
- Family history of breast or ovarian cancer
- Known BRCA1 (Breast Cancer gene 1) or BRCA2 (Breast Cancer gene 2) mutations
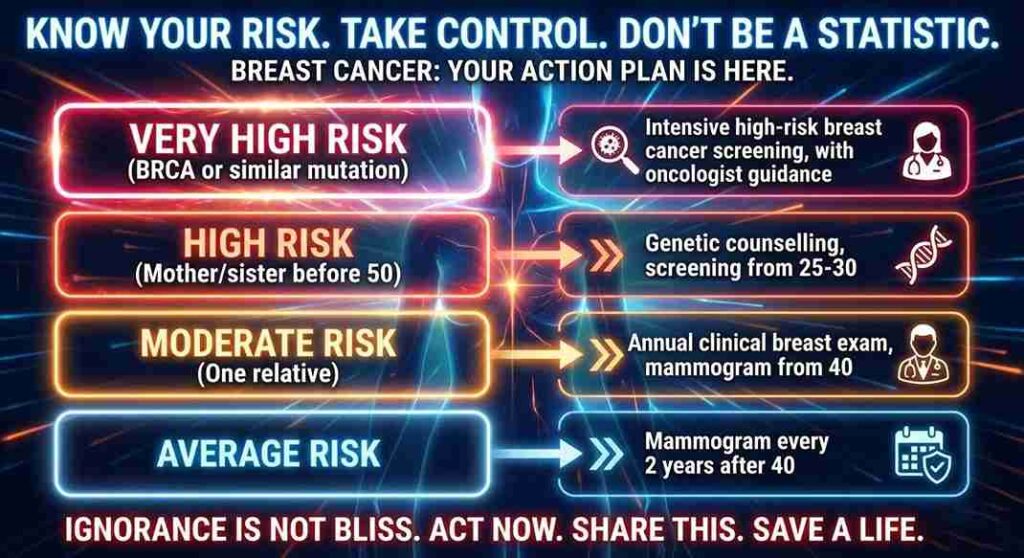
How Do You Know Which Breast Cancer Risk Category You Fall Into?
Risk level is determined by family history, age of diagnosis in relatives, and genetic test results. Screening intensity increases with the risk category.
What Is Hereditary Breast Cancer and Which Genes Are Responsible?
Hereditary breast cancer occurs due to faulty DNA-repair genes such as BRCA1 or BRCA2, or TP53 (Tumour Protein 53).
These mutations significantly raise lifetime cancer risk and require early screening.
- About 5–10 % of all breast cancers are hereditary. (Source)
- If your mother or sister had breast or ovarian cancer before age 50, doctors recommend genetic testing for breast cancer.
- BRCA gene testing in Kolkata is widespread – a simple blood or saliva test that can tell you if you carry the mutation.
“A half-hour test can give you years of mental peace,” –Dr Suvadip Chakrabarti. “The goal is knowledge, not anxiety.”
Which Breast Cancer Screening Tests Save Lives the Most?
Screening tests detect cancer years before symptoms appear. Early detection allows simpler treatment and significantly improves survival rates.
Many women skip screening because they’re busy. Morning puja, office work, cooking, managing the household—where’s the time?
But breast cancer screening tests detect changes years before symptoms appear. Catching cancer early means simpler treatment and better survival.
At What Age Should Breast Cancer Screening Begin If There Is a Family History?
Screening usually starts 10 years before the age at which the youngest affected relative was diagnosed, but not earlier than age 25.
Clinical Breast Examination:
- The doctor examines the breasts by hand, checking for lumps
- Every year, from age 2,5 if you havea family history
- Takes 10-15 minutes with any breast specialist doctor in Kolkata
Mammography Test:
- A low-dose X-ray that takes pictures of breast tissue
- From age 40 annually; earlier (age 30-35) if high risk
- Detects tiny tumours you can’t feel yet
- Available across Kolkata from Alipore to Salt Lake
Ultrasound and MRI:
- Ultrasound uses sound waves, perfect for dense breast tissue
- MRI for high-risk women with BRCA mutations
- Your doctor decides based on your risk profile
Which Breast Cancer Screening Test Is Right for Your Risk Level?
Mammography suits average-risk women, while ultrasound and MRI are used for dense breasts and high-risk genetic cases. Test choice depends on individual risk profiling.
| Test | Starting Age | Frequency | Best For |
| Self-exam | From age 20 | Monthly | Everyone |
| Clinical exam | From age 25-30 | Yearly | Family history |
| Mammogram | Age 40 (or 30 if high-risk) | Every 1-2 years | All women over 40 |
| MRI | Age 25-30 | Yearly | Very high-risk, BRCA+ |
You get modern diagnostics, including mammography tests, where digital machines can spot tumours as small as a grain of rice—long before they’re felt.

What Are the Early Signs of Breast Cancer You Should Never Ignore?
New lumps, skin dimpling, nipple discharge, breast shape changes, or persistent pain require immediate medical evaluation—even if symptoms seem mild.
Every month after your period, examine your breasts. Stand before the mirror. Look. Feel. Notice.
Many women dismiss symptoms as “hormonal” or “normal.” Yet awareness saves lives.
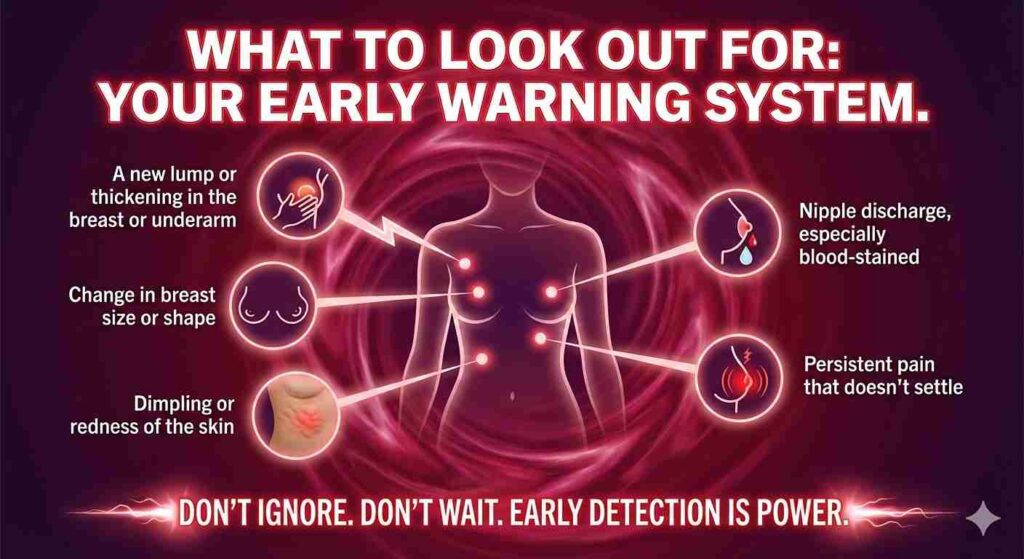
The early signs of breast cancer are often subtle—but catching them early means almost 100 % survival – [Source]
Are Most Breast Lumps Cancerous?
Most breast lumps are benign. However, only clinical examination and imaging can determine whether a lump is cancerous.
If you notice anything unusual, visit a leading breast cancer doctor in Kolkata immediately.
Early detection changes everything. Most breast cancers caught at Stage 1 have a very high five-year survival rate.
Can Lifestyle Changes Reduce Breast Cancer Risk Despite Family History?
Regular exercise, weight control, limiting alcohol, not smoking, breastfeeding, and timely screening can reduce breast cancer risk by up to 10–15 years.
What Should Be Your Family History Breast Cancer Prevention Checklist?
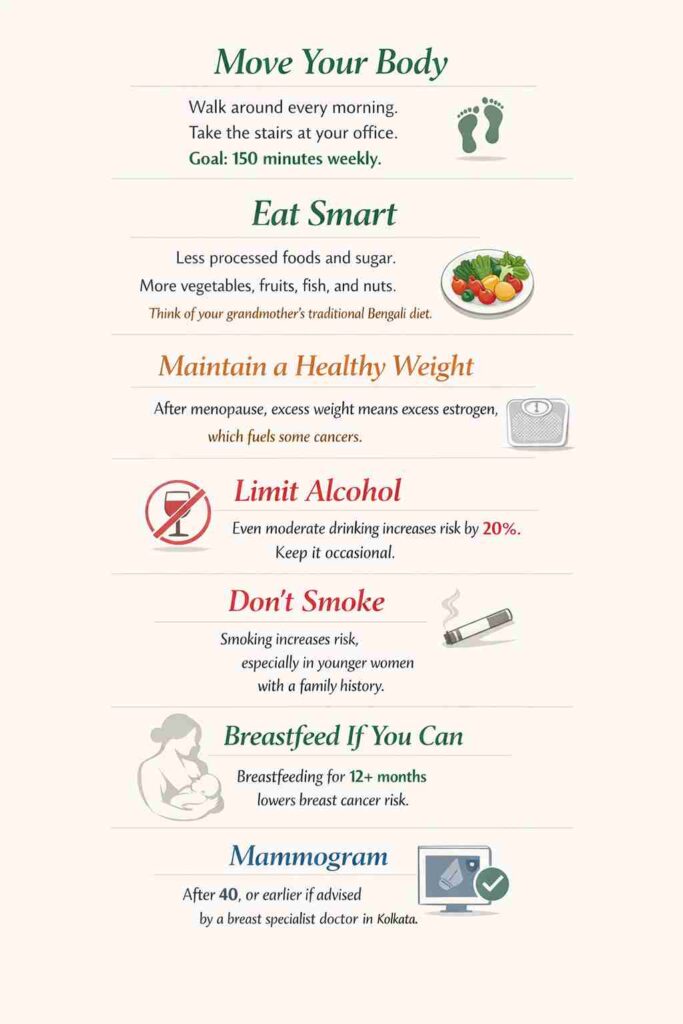
Your genes may set the risk. But your lifestyle decides the timing.
Healthy habits can delay the onset of cancer by 10-15 years.
[Source]
Does Having a Family History Mean Your Outcome Will Be the Same?
Family history does not determine outcome. Early awareness, genetic testing, and structured screening allow prevention or early-stage detection with excellent survival rates.
Having a family history doesn’t mean having cancer. Knowing your risk helps you act rather than panic.
Your mother or aunt may not have had access to genetic testing or expert guidance. But you do. This is to your advantage.
When Should You Consult a Breast Cancer Specialist?
Consult a specialist if there is a family history, genetic risk, new symptoms, or uncertainty about screening timelines. Early consultation improves clarity and outcomes.
Your Story Doesn’t Have To Be the Same as Your Predecessors’.
📞Consult Dr Suvadip Chakrabarti today, a renowned breast cancer doctor in Kolkata.
People Also Ask
Does family history mean breast cancer is inevitable?
No. Family history increases risk but does not guarantee breast cancer. Most women with affected relatives never develop the disease.
When should breast cancer screening start with a family history?
Screening should begin 10 years before the age at which the youngest close relative was diagnosed, but not earlier than age 25.
Who should consider BRCA genetic testing?
BRCA testing is advised if a mother, sister, or close relative had breast or ovarian cancer before age 50.
How often should mammograms be done in high-risk women?
High-risk women usually require annual mammograms starting between the ages of 30 and 40, based on medical advice.
Can lifestyle changes lower hereditary breast cancer risk?
Yes. Regular exercise, weight control, limited alcohol, and timely screening can significantly reduce overall risk.


