The vulva of women is affected by vulvar cancer, which is a rare type of cancer. It should not be confused with the vagina. The folds of skin that protect the vaginal and urethral openings are the labia majora and labia minora and these make up the vulva.
In vulval cancer, there are several types and among them, the most common is squamous cell vulvar carcinoma. Among the diagnosed cases, it accounts for more than 90%. The second most common is melanoma of the vulva and among those women with vulvar cancer, it represents about 5%. There are different other types also. Paget’s Disease of the vulva, vulvar adenocarcinoma, and basal cell carcinoma are some of them, which are much less common.
Causes and Risk Factors of Vulvar Cancer
The known risk factors for the disease have been identified by researchers, although they have yet to pinpoint the exact causes of vulvar cancer. Some of the risk factors for vulvar cancer according to oncologists are:
• Getting infection from HPV (human papillomavirus)
• Getting infection from HIV
• A skin condition called lichen sclerosis that affects the vulva
• Habit of smoking
• Having a history of melanoma in the family
• Age of 70 years or over (however, in younger women also, vulvar cancer can be diagnosed)
Symptoms of Vulvar Cancer
There are rarely any symptoms of vulvar cancer in the early stages. The symptoms of vulvar cancer are seen as the disease progresses. They are:
• The presence of a lump or bump on the vulva
• Having itching, burning, or sensitivity in the vulva
• During urination, there is a feeling of pain
• In the texture of the vulva, a change is seen
• On the vulva, a mole develops or there is a change in an existing mole
• No relation between any bleeding and your menstrual cycle
There can be a relation of these vulvar cancer symptoms to another, less serious condition. These symptoms are not only exclusive to vulvar cancer. It may help in early detection if you report these symptoms to your doctor.
Diagnosis of Vulvar Cancer
Your cancer doctor should be aware of any symptoms experienced by you. In diagnosing vulvar cancer, this is the first step. Women may visit their doctor on seeing the symptoms, but through routine pelvic exams, signs of vulvar cancer can be detected, even if a woman is not experiencing any noticeable symptoms.
If women do regular vulvar self-examinations at home, they can monitor their vulvar health. If these exams are regularly done by a woman, she can understand her anatomy, learn what is normal for her vulva, and over time, possible abnormal changes that could indicate an abnormality.
In order to confirm the presence or absence of cancer, a biopsy is needed. The best gynae oncologist removes a small sample of vulvar tissue during a vulvar biopsy and this is sent to a pathology lab for screening. The disease is staged when a biopsy reveals cancer. The extent, to which cancer has spread to nearby tissues or organs, is referred to by staging. In diagnosing vulvar cancer, other tests are also used. Some of these are:
• Cystoscopy
• Proctoscopy
• X-ray examination of the lungs
• Intravenous urography (as needed)
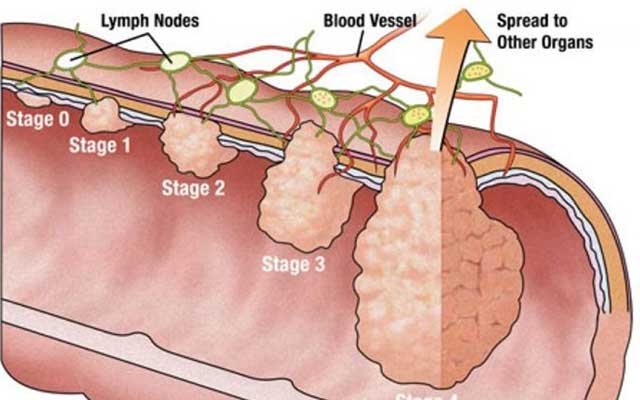
Stages of Vulvar Cancer
• Stage I. In the vulva or perineum, the area of skin between the vaginal opening and anus, there is a small tumour. At this stage, your lymph nodes or other areas of the body are not affected by cancer.
• Stage II. The lower portions of the urethra, vagina and anus are affected by the tumours in this stage.
• Stage III. In this stage, the lymph nodes are affected by cancer.
• Stage IV. The lymph nodes, upper portions of the urethra or vagina, bladder, rectum or pelvic bone are affected by cancer in this stage.
Treatment of Vulvar Cancer
The stage of cancer and general health plays an important role in deciding vulvar cancer treatment plans. Surgery, chemotherapy and radiation therapy are the three methods used to treat vulvar cancer.
Among the different types of vulvar cancer treatment, surgery is the most common. During local excision, one type of surgery, the cancerous tissue is removed by the best surgical oncologist along with a margin of healthy tissue surrounding it. If necessary, lymph nodes may be removed.
For some women, a vulvectomy, another surgical procedure is used. The removal of all or part of the vulva and is reserved for more advanced cases of vulvar cancer is involved in it.